-
Recent Posts
Archives
- October 2022
- August 2022
- May 2022
- March 2022
- January 2022
- December 2021
- September 2021
- July 2021
- June 2021
- May 2021
- April 2021
- February 2021
- January 2021
- November 2020
- October 2020
- September 2020
- June 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- June 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- August 2016
- July 2016
- June 2016
- May 2016
- April 2016
- March 2016
- February 2016
- January 2016
- December 2015
- November 2015
- October 2015
- September 2015
- August 2015
- July 2015
- June 2015
- May 2015
- April 2015
- March 2015
- December 2014
- June 2014
- May 2014
- April 2014
- November 2013
- September 2013
- August 2013
- July 2013
- June 2013
- May 2013
- March 2013
- January 2013
- November 2012
- October 2012
- July 2012
- December 2011
- November 2011
- October 2011
- September 2011
- August 2011
- July 2011
- June 2011
- May 2011
- April 2011
- March 2011
- February 2011
- January 2011
- December 2010
- November 2010
Categories
Pulmonic Stenosis and Balloon Valvuloplasty in Dogs
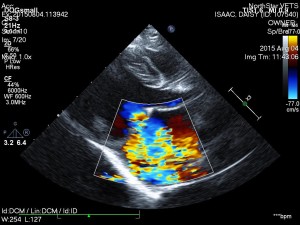
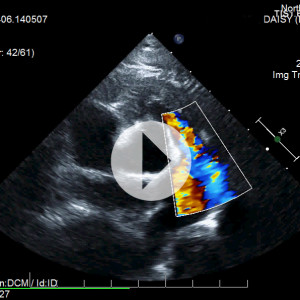
Daisy is a 10-month-old, female English bulldog who was diagnosed with severe congenital heart disease called pulmonic stenosis. This condition can lead to congestive heart failure and a poor long-term prognosis if left untreated. Fortunately, we were able to perform a balloon valvuloplasty (cardiac catheterization procedure) at NorthStar VETS to help improve her heart function and quality of life!
The information presented on this web site is not intended to take the place of your family veterinarian’s advice and is not intended to diagnose, treat, cure or prevent any disease. Discuss this information with your own veterinarian to determine what is right for your pet. All information is intended for your general knowledge only and is not a substitute for medical advice or treatment for specific medical conditions. We can not and do not give you medical advice via this blog. The information contained in this online site and emails is presented in summary form only and intended to provide broad understanding and knowledge. The information should not be considered complete and should not be used in place of a visit, call, consultation or advice of your veterinarian. We do not recommend the self-management of your pet’s health problems.
Pulmonic stenosis, known as PS, is one of the most common congenital heart diseases in dogs. It can be accompanied by additional heart defects and develop into a life-threatening condition or it can be mild enough to be no more than a surprising incidental finding. Pulmonic stenosis refers to a stenosis or constriction of the right ventricular outflow tract.
Pulmonic stenosis is most commonly seen in English bulldogs like Daisy, as well as Terriers, Miniature Schnauzers, American Cocker Spaniels, Samoyeds, Keeshounds, Mastiffs and Beagles. A hereditary bases for PS has been proven in Beagles and is suspected in other breeds.
 In order to understand what pulmonic stenosis is, it is necessary to understand some normal heart anatomy. The heart sits more or less centrally in the chest and is divided into a left side, which receives oxygen-rich blood from the lungs and pumps it to the rest of the body; and a right side, which receives “used” blood from the body and pumps it to the lungs to pick up fresh oxygen. Because the left side of the heart must supply blood to the whole body, its muscle is especially thick and strong while the right side, which only pumps to one nearby area, tends to be thinner. When the ventricles pump, the blood from the left shoots through the aortic valve and the blood from the right side shoots through the pulmonic valve. These valves snap sharply closed after the pumping is done. The area where the blood exits the right ventricle is called the right ventricular outflow tract and it consists of the exit area of the ventricle, the pulmonic valve, and the main pulmonary artery.
In order to understand what pulmonic stenosis is, it is necessary to understand some normal heart anatomy. The heart sits more or less centrally in the chest and is divided into a left side, which receives oxygen-rich blood from the lungs and pumps it to the rest of the body; and a right side, which receives “used” blood from the body and pumps it to the lungs to pick up fresh oxygen. Because the left side of the heart must supply blood to the whole body, its muscle is especially thick and strong while the right side, which only pumps to one nearby area, tends to be thinner. When the ventricles pump, the blood from the left shoots through the aortic valve and the blood from the right side shoots through the pulmonic valve. These valves snap sharply closed after the pumping is done. The area where the blood exits the right ventricle is called the right ventricular outflow tract and it consists of the exit area of the ventricle, the pulmonic valve, and the main pulmonary artery.
In pulmonic stenosis, the right ventricular outflow tract is narrowed either at the actual valve, just before it, or just after it. The most common form of pulmonic stenosis involves a deformed pulmonary valve such that the valve leaflets are too thick, the valve cusps are fused, or the opening is too narrow such as in the formation of an aberrant coronary artery. The heart must pump extra hard to get the blood through this unusually narrow, stiff valve. The right side of the heart becomes thick from all this extra work which may result in abnormal electrical conduction of the heart, leading to arrhythmias. In some cases these arrhythmias can be life-threatening.
A mild case is of little concern and usually does not affect life expectancy. Luckily, most cases are mild and do not require treatment; fairly severe disease is needed for clinical signs to appear.
Approximately 35-percent of dogs with severe pulmonic stenosis will show some or all of the following signs:
- Tiring easily
- Fainting spells (from the abnormal electrical heart rhythm)
- Fluid accumulation in the belly
- Blue-tinge to the gums, especially with exertion
- Difficulty breathing
- Sudden death
In some cases, medications called beta blockers can be used in an attempt to relax the muscles of the heart and open the stenosis. This will not relieve the constriction but could relieve it. In mild forms of the disease, medical management may offer the pet a good quality of life.
Clearly, if the obstruction at the pulmonic valve could be relieved, much of the problem would be solved. Severe pulmonic stenosis cases can be treated by doing just that. A special balloon is inserted into the pulmonic valve where it is inflated, breaking down the obstruction. The size of the balloon catheter is determined by echocardiography as described above. Dogs that have severe pulmonic stenosis should have this procedure regardless of whether or not they are showing clinical signs.Performing this procedure reduces the risk of sudden death by 53-percent and improves quality of life as well. However, certain types of valve deformity are not amenable to this treatment.
If your family veterinarian believes your pet needs to see a specialist, contact NorthStar VETS at 609.259.8300 to schedule an appointment with one of our veterinary specialists.
 Jennifer Schneiderman, DVM, DACVIM (Cardiology)
Jennifer Schneiderman, DVM, DACVIM (Cardiology)
Dr. Schneiderman received her Doctorate of Veterinary Medicine degree at Ross University in 2009 before moving back home to Long Island, New York where she completed a one-year rotating internship in small animal medicine and surgery at Atlantic Coast Veterinary Specialists in March 2010. After that, she completed a three-year residency in Cardiology at Atlantic Coast Veterinary Specialists in July 2013 and then stayed on there as a Staff Cardiologist until June 2014. Now a board-certified Veterinary Cardiologist, Dr. Schneiderman joined the NorthStar VETS team in August 2014. Her clinical interests include treatment of congestive heart failure and complex arrhythmias along with an interest in interventional procedures such as pacemaker implantation, balloon valvuloplasty and patent ductus arteriosus occlusion. Outside of work, Dr. Schneiderman enjoys traveling, scuba diving, going to the beach and spending time with her two tuxedo cats.
The information presented on this web site is not intended to take the place of your family veterinarian’s advice and is not intended to diagnose, treat, cure or prevent any disease. Discuss this information with your own veterinarian to determine what is right for your pet. All information is intended for your general knowledge only and is not a substitute for medical advice or treatment for specific medical conditions. We can not and do not give you medical advice via this blog. The information contained in this online site and emails is presented in summary form only and intended to provide broad understanding and knowledge. The information should not be considered complete and should not be used in place of a visit, call, consultation or advice of your veterinarian. We do not recommend the self-management of your pet’s health problems.
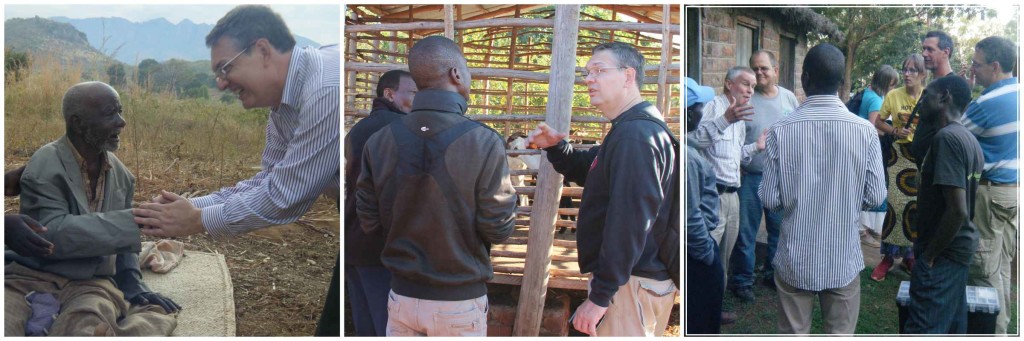
VIP Brings Hope and Healing to Malawi this Summer
This past July, NorthStar VETS was back in Malawi, Africa to check up on the villagers our team had been helping there. Here is the summary report from Villages in Partnership.
“NorthStar VETS sent its Theriogenologist, Dr. Manoel Tamassia, to work with farmers and their livestock. He was joined by Pat Boland, veternarian for National Rural Poultry Centre in Malawi, along with others to discuss best practices. It is challenging to convince a farmer to care for an animal when their family is hungry. Feeding livestock will pay off in the long term, but long term planning is not a mindset when short term circumstances are dire.”
“NJ State apiarist, Tim Schuler, returned to Malawi, thanks once again to NorthStar VETS. He continued to learn from, work and share knowledge with Malawian bee keepers. They harvested much honey and all enjoyed the spoils.”

The mission of Villages in Partnership is to build partnerships between villages in the developed world and villages in Malawi to bring about life-changing development for all. The organization works with local development experts in Malawi to implement programs designed to simultaneously address the inter-connected web of root causes of extreme poverty: lack of access to clean water, food insecurity, poor health care, inadequate education, insufficient infrastructure, and lack of economic opportunities.
 Manoel Tamassia, DVM, MS, Ph.D, DACT
Manoel Tamassia, DVM, MS, Ph.D, DACT
Dr. Tamassia left engineering school to attend veterinary school at the Universidade Estadual de Londrina, Brazil, where he graduated in 1989. With a strong interest in animal reproduction, he moved to Columbia, Missouri to start an internship in theriogenology, continuing his training by completing a residency in theriogenology and a master of science degree in reproductive physiology. Dr. Tamassia remained at the University of Missouri College of Veterinary Medicine as an assistant instructor, during which time he completed the requirements for the ECFVG program (DVM equivalency for foreign graduates). He then moved to the University of Illinois, College of Veterinary Medicine working in the production animal and theriogenology section for three years.
Dr. Tamassia returned to Brazil in 1997 where he practiced and taught large-animal reproduction until he moved to Paris, France to continue his education at the Institut National Agronomique de Paris. For four years he worked with in-vitro fertilization and cloning, finishing his graduate studies and PhD in 2003. He returned to the U.S. to be an assistant professor in theriogenology at the College of Veterinary Medicine at the University of Illinois. In 2009, he was awarded Diplomate status in the American College of Theriogenology and joined NorthStar VETS, where he provides comprehensive reproductive medical services for all species. Dr. Tamassia also serves as the State Veterinarian for NJ under Governor Christie and oversees the NJ State Animal Health Diagnostic Lab.
Posted in Veterinary Medicine
Tagged Africa, humanitarian, Malawi, Manoel Tamassia, NorthStar VETS, Theriogenology, Villages in Partnership
Leave a comment
The Story of Oliver
 Oliver NorthStar, who is now about two-and-a-half years old, is our male, neutered, domestic short-hair, hospital cat. Ollie first came to us as a kitten on June 5th, 2013 at approximately two months of age. A Good Samaritan had found him and brought him here, even though we do not generally accept these types of cases.
Oliver NorthStar, who is now about two-and-a-half years old, is our male, neutered, domestic short-hair, hospital cat. Ollie first came to us as a kitten on June 5th, 2013 at approximately two months of age. A Good Samaritan had found him and brought him here, even though we do not generally accept these types of cases.
On presentation, it was clear that he had a bad upper respiratory infection and gastrointestinal problems. When examined, we noted that (despite being stray) he was very tame and easily handled, but had moderate nasal discharge, was sneezing with some harsh upper airway noise, and had some bloody stool suspicious for parasites or other intestinal infection. Despite his issues, he was a really nice cat! We treated him initially for his upper respiratory infection and waited to see if he had an owner who missed him. He was never claimed.
 After a few days, he was hospitalized and given some basic supportive care for his symptoms while we attempted to contact the local Animal Control with the hope that they would pick him up for transport to a local shelter for continued care. Unfortunately, Animal Control was unable to take him. We debated for some time about dropping him off at a local shelter ourselves, but were unable to find one that had room to take him.
After a few days, he was hospitalized and given some basic supportive care for his symptoms while we attempted to contact the local Animal Control with the hope that they would pick him up for transport to a local shelter for continued care. Unfortunately, Animal Control was unable to take him. We debated for some time about dropping him off at a local shelter ourselves, but were unable to find one that had room to take him.
We felt strongly that he had a good prognosis with some time and TLC, so Oliver continued to sit in our care for several weeks. Luckily, his symptoms resolved with treatment. After being here for more than a month, he started becoming a part of the family with his sweet temperament and affectionate nature. Many of us got attached to this adorable cat with an amazing personality, so we decided to treat him extensively for the problems he had. After much pleading from the entire staff, our Chief of Staff, Dr. Stobie, agreed to let us keep him as a hospital cat and become the new mascot for NorthStar VETS.
 After a course of antibiotics, he improved, but his upper respiratory signs did not resolve completely. There was still one more health challenge for him to overcome. He was diagnosed with a nasopharyngeal polyp which was removed by our team. After two months of being a foster, he was finally transitioned into being our hospital cat.
After a course of antibiotics, he improved, but his upper respiratory signs did not resolve completely. There was still one more health challenge for him to overcome. He was diagnosed with a nasopharyngeal polyp which was removed by our team. After two months of being a foster, he was finally transitioned into being our hospital cat.
At this time, he had no official name, and that is where our extended family of clients came in. We held a two-part social media contest to come up with names for the new guy, and then vote on the best one. Oliver NorthStar was the winning name, and the rest is history.
 For those who remember Robbie, our long-time hospital cat prior to Oliver, you will remember he was a good ambassador in our lobby. He would greet every client and seemed to have no fear of dogs. Oliver has filled that role perfectly. You will often find him staring at leaves out the window, basking in the sun on the waiting room couches, or hanging out in pharmacy. You may even catch him trying to sneak into the back of the hospital searching for treats. His favorite hobbies are to watch birds in the waiting room and stalk other cat carriers. If a cat carrier is open, he will walk in and take a nap. Or he will sit on top of a cat carrier when one of our patients is waiting to be seen. He has even been so bold as to take advantage of a client crocheting by sleeping in her project while she worked!
For those who remember Robbie, our long-time hospital cat prior to Oliver, you will remember he was a good ambassador in our lobby. He would greet every client and seemed to have no fear of dogs. Oliver has filled that role perfectly. You will often find him staring at leaves out the window, basking in the sun on the waiting room couches, or hanging out in pharmacy. You may even catch him trying to sneak into the back of the hospital searching for treats. His favorite hobbies are to watch birds in the waiting room and stalk other cat carriers. If a cat carrier is open, he will walk in and take a nap. Or he will sit on top of a cat carrier when one of our patients is waiting to be seen. He has even been so bold as to take advantage of a client crocheting by sleeping in her project while she worked!
 So next time you come to NorthStar VETS, make sure to look for Ollie and say hello!
So next time you come to NorthStar VETS, make sure to look for Ollie and say hello!
 Jennifer Kim, DVM, DACVIM (Oncology)
Jennifer Kim, DVM, DACVIM (Oncology)
Dr. Kim grew up in New York and received her BA from the University of Pennsylvania. After two years at the National Cancer Institute performing cancer genetic research, she attended veterinary school at Tufts University. Dr. Kim completed a rotating internship at the Animal Medical Center in Manhattan, New York, and an oncology internship at Cornell University. She began at NorthStar VETS as an emergency clinician in 2005 and returned in 2010 to treat oncology patients after completing her residency in medical oncology at Michigan State University School of Veterinary Medicine. In her free time, Dr. Kim is an avid foodie and knitter.
 Stacey Rebello, DVM, MS
Stacey Rebello, DVM, MS
Dr. Rebello is a New Jersey native who completed her undergraduate degree in biology at Fairfield University while working as a technician at a local veterinary clinic. She earned a master of science degree in theriogenology, studying equine placentitis and placental drug transfer at the University of Florida. She continued her studies at UF and was awarded her doctor of veterinary medicine degree in 2008. Dr. Rebello returned to New Jersey for an internship in small animal medicine and surgery at Garden State Veterinary Specialists in Tinton Falls. She joined the NorthStar VETS emergency department in 2009, where her clinical interests include trauma care and perioperative management of surgical emergencies.
Posted in Pets
Tagged hospital cat, Jennifer Kim, NorthStar VETS, Oliver, Stacey Rebello
Leave a comment
Ask the NorthStar VETS Vet: Heart Murmurs in Dogs and Cats
My pet has a heart murmur – what does this mean?
A heart murmur is one of several types of abnormal sounds your veterinarian can hear when listening to your pet’s heart with a stethoscope. Normally, two distinct sounds are heard when listening to the heart of a normal dog or cat. These are often described as “lub” and “dub.” When listening with a stethoscope one hears: Lub-dub…Lub-dub….Lub-dub.
A murmur is an abnormal extra sound (which can sometimes drown out the normal sounds). Murmurs most commonly occur between the “lub” and the “dub” and have a “shooshing” or “whooshing” quality.
Hearing a heart murmur during a routine physical examination will often be the first hint to your veterinarian that your pet has heart disease. Hearing a murmur is only a hint that something may be wrong (a clinical sign), not a final diagnosis. Hearing a murmur is reason to consider more discussion and tests to determine the cause of the murmur (the diagnosis). Knowing the diagnosis and severity of the cause of the murmur allows your veterinarian (or a cardiologist they consult) to provide you with an educated guess (prognosis) regarding how this heart problem may affect your pet in the future.
Hearing a murmur is not a reason to panic. Many dogs and cats with murmurs live normal lives and never need any treatment for heart disease. But the only way to know for certain is to work with your veterinarian to determine the cause and severity of the cause of the murmur.
What causes a heart murmur?
The short answer to this question is “turbulent blood flow.” Like the water in a calm river or stream, blood flowing normally flows through the heart with laminar flow – that is, it is smooth and undisturbed. And like a river or stream, narrowing, or other causes of more rapid flow, will disrupt this smooth laminar flow. In a river the turbulent rapids emit sounds much louder and less tranquil than the calmer sections of river. In the heart we hear this turbulence as a murmur.
Murmurs caused by abnormalities of the heart can be due to:
- Valvular diseases
- A narrowing (stenosis) within a chamber or vessel through which the blood has to “squeeze” through, like water through a pinched hose
- A “hole in the heart” between two chambers or two arteries that are not normally connected
- A thicker than normal heart muscle
What is a benign or “innocent” murmur?
Some heart murmurs are called benign (or innocent or physiological), meaning there is no apparent heart disease that explains the murmur. These murmurs are often seen in puppies, and can occur in cats of any age. They are uncommon in adult dogs. Benign murmurs are usually soft (rather than loud), and can be intermittent. Benign puppy murmurs will generally disappear by 12 to 15 weeks of age. Murmurs associated with anemia or excitement are also considered benign murmurs.
What is a congenital murmur vs. an acquired murmur?
A congenital murmur is a murmur in a pet that is present from birth (or near birth). Congenital murmurs are associated with heart defects that the pet was born with. However, some congenital murmurs may be missed in puppies or kittens and only detected later in life. An acquired murmur is a murmur that a pet acquires during their life. These can be benign, but more often (especially in dogs) are associated with developing heart or valve disease.
My pet’s murmur has a “grade.” What does this mean?
Murmur grading is simply your veterinarian’s way of describing the loudness of a murmur. There are six murmur grades. The lower the grade, the quieter the murmur. However, it is often easiest to simply describe them as “soft,” “moderate,” or “loud.” There are other terms that a vet will use to describe the character of a murmur – this helps communicate to other veterinarians the characteristics of the murmur as certain types of murmurs are more commonly associated with specific heart or valve diseases.
The grade or loudness of the murmur is only sometimes related to the severity of the heart abnormality causing it. Bear in mind that grading is subjective because it is based on how it sounds to the listener. Also, it’s hard to tell if an animal has a heart murmur if the pet is excited or anxious, because rapid breathing sounds can mimic a murmur. Usually, only a trained cardiologist can identify a Grade 1 murmur. A Grade 5 or Grade 6 murmur is so strong that it can be felt through the chest wall (like water being sprayed against a sheet of cloth).
What should I do if my pet has a murmur?
Dogs
In many cases, a veterinarian will be able to determine the likely cause of a murmur in a dog just by listening. In some cases, no additional testing will be deemed necessary. However, to be certain, it is often best to work with your veterinarian to confirm the cause of the murmur as well as the severity of the condition that is causing the murmur. This will give you the best idea of what to expect in the future — the prognosis for your pet. In other cases, where a pet may be used for breeding, a murmur may indicate the presence of a hereditary defect that could be passed on to progeny.
Cats
The cause of a cat’s murmur cannot usually be determined by listening alone. In many cats, benign murmurs can sound exactly like murmurs in a cat with serious heart disease.
In both dogs and cats, your veterinarian may elect to perform chest radiographs (x-rays), an echocardiogram (ultrasound of the heart), or other imaging studies, or to refer your pet to a specialist for these procedures. The tests that are performed depend on the individual case.
How is a murmur treated?
The murmur itself is not treated. The underlying cause of the murmur may or may not be treated – this depends on the cause, severity, and other circumstances (age, well-being of the pet, cost of treatment etc). Your veterinarian is best-suited to discuss specific treatment options with you.
If your pet needs to see a veterinary Cardiologist in our Cardiology service, call NorthStar VETS at 609.259.8300. Once your appointment is set, you may complete your Cardiology pre-appointment paperwork.
 Jennifer Schneiderman, DVM, DACVIM (Cardiology)
Jennifer Schneiderman, DVM, DACVIM (Cardiology)
Dr. Schneiderman received her Doctorate of Veterinary Medicine degree at Ross University in 2009 before moving back home to Long Island, New York where she completed a one-year rotating internship in small animal medicine and surgery at Atlantic Coast Veterinary Specialists in March 2010. After that, she completed a three-year residency in Cardiology at Atlantic Coast Veterinary Specialists in July 2013 and then stayed on there as a Staff Cardiologist until June 2014. Now a board-certified Veterinary Cardiologist, Dr. Schneiderman joined the NorthStar VETS team in August 2014. Her clinical interests include treatment of congestive heart failure and complex arrhythmias along with an interest in interventional procedures such as pacemaker implantation, balloon valvuloplasty and patent ductus arteriosus occlusion. Outside of work, Dr. Schneiderman enjoys traveling, scuba diving, going to the beach and spending time with her two tuxedo cats.
The information presented on this web site is not intended to take the place of your family veterinarian’s advice and is not intended to diagnose, treat, cure or prevent any disease. Discuss this information with your own veterinarian to determine what is right for your pet. All information is intended for your general knowledge only and is not a substitute for medical advice or treatment for specific medical conditions. We can not and do not give you medical advice via this blog. The information contained in this online site and emails is presented in summary form only and intended to provide broad understanding and knowledge. The information should not be considered complete and should not be used in place of a visit, call, consultation or advice of your veterinarian. We do not recommend the self-management of your pet’s health problems.
Dogs and Children Bond at Best Friends Bash
On September 11, 2012, I gave a lecture to a roomful of medical doctors, including plastic surgeons, oral and maxillofacial surgeons, otorhinolaryngologists, psychologists, nurses and other caretakers of children born with craniofacial defects as part of a lecture series at the Edwin and Fannie Gray Hall Center for Human Appearance. The topic of my lecture was “Functional and Esthetic Considerations of Maxillofacial Reconstruction in Companion Animals.” To conclude the lecture, I suggested that it would be great to bring our craniofacial veterinary patients together with children who are dealing with similar craniofacial conditions. This gathering came together (due to a lot of hard work by Diana Sweeney from CHOP) on July 17, 2013, and was named the “Best Friends Bash.” The interactions between the young CHOP patients and our veterinary patients were nothing less than magical.
Pets and people are often affected by the same illnesses. Treatment for those illnesses is often remarkably similar. Craniofacial deformities can be some of the most challenging diseases for a patient to cope with, due to stigmas associated with facial differences. Many of these deformities are congenital in nature, and in humans, multiple surgeries are often necessary to improve function and cosmetics. It is not uncommon for some patients to require over 30 surgeries throughout life if born with severe congenital craniofacial deformities. Therefore, human patients may need to spend much of their time in the hospital for procedures and recheck examinations. These visits can be made much more palatable if there is a four-legged friend awaiting one’s arrival. The bond created is even more special when the dog shares a common ailment with the child.
Dogs have always inspired me with their ability to not shy away from adversity, to not dwell on negative aspects of their lives and to not worry about those things they cannot control (at least as far as we can tell!). In speaking with some of the doctors and patient caretakers at the Children’s Hospital of Philadelphia, it seems children with craniofacial defects are equally inspiring.
A few years ago, I met a 29-year-old woman named Jaci at the gathering. Jaci was born with Apert syndrome, an inherited autosomal dominant condition. It is caused by mutations in the gene that codes for fibroblast growth factor receptor 2. This gene defect causes craniosynostosis, where some of the bony sutures of the skull close too early. Symptoms include early closure of sutures between bones of the skull, as seen by ridging along sutures; frequent ear infections and hearing loss; fusion or webbing of the second, third, and fourth fingers and toes; prominent or bulging eyes; severe under-development of the mid-face; and limb length abnormalities. Though Jaci is now 32, she often attends gatherings like the “Best Friends Bash” because doctors and caretakers at the Children’s Hospital of Philadelphia have become family to her throughout the years. After multiple surgeries, Jaci has become comfortable with her function and appearance. She feels canine therapy dogs, especially dogs who had craniofacial procedures themselves, “will be great for kids born with Apert syndrome, cleft lip and cleft palate since the kids can see how well the dogs do with their differences.” The Best Friends Bash allows us to catch up with both canine and human friends made during past events.Last week marked the third annual Best Friends Bash. The magic continues to be palpable and the dogs continue to brighten the room! And with the help of corporate sponsorship, it looks like the Best Friends Bash will go national in the near future. Another example of the healing power of pets!

John Lewis, VMD, FAVD, DAVDC
Dr. John Lewis is the veterinary dentist at NorthStar VETS. He was Assistant Professor of Dentistry and Oral Surgery at the University of Pennsylvania. He graduated from University of Pennsylvania School of Veterinary Medicine in 1997 and spent 5 years in general practice prior to returning for a residency in dentistry and oral surgery. Dr. Lewis became a fellow of the Academy of Veterinary Dentistry (AVD) in 2004 and a diplomate of the American Veterinary Dental College (AVDC) in 2005. At the University of Pennsylvania, Dr. Lewis has served as Associate Director of the Mari Lowe Center for Comparative Oncology, and more recently, as Chief of Surgery. Dr. Lewis’ research interests include oral surgical oncology, maxillofacial fracture repair, maxillofacial reconstruction, new therapies for treatment of feline oral squamous cell carcinoma, and lasers in oral surgery and dentistry. Dr. Lewis is a past President of the American Veterinary Dental Society, and has served as Examination Chair of the AVDC and Credentials Chair of the AVD. Prior to joining NorthStar VETS full-time, Dr. Lewis was the residency director of the world’s first academic residency in Veterinary Dentistry and Oral Surgery at Penn Vet.
Posted in Pets
Tagged childrens hospital of Philadelphia, craniofacial deformities, Dogs, john lewis, NorthStar VETS
Leave a comment
Breathing Issues in Cats
We often get questions from our clients about how to tell if your cat is breathing alright or not. On this blog, I have attached two videos of my cats having trouble breathing (dyspnea) for two different reasons.
Cats can have issues breathing due to many problems. Most commonly, we see young cats with asthma, any age cat with anemia, and older cats with fluid around their lungs. As you watch these videos you can see that they are quite similar. Look at the abdomen. You will notice when they breathe in and out, it is with the abdomen. This is not normal. And you can see that both cats are at rest. If you look at their gums, you might notice that they do not look the same pink color they should, but look either pale or slightly blue/purple.
Rocco, sitting on the blanket, was having trouble breathing because he was very anemic (low red blood cell count) (click link to see video). His gums were pale. He was weak and lethargic. Sadly, I said goodbye to Rocco the day after I took this video.
Norman Rat Baits, the tabby on the floor, was dyspneic due to asthma (click link to see video). He was only slightly lethargic, still eating, and acting relatively normal. Norman would also occasionally cough, and when his breathing got worse, would open his mouth and breathe like a panting dog. Norman is doing great with his asthma treatments and is back to being his usual crazy self.
When cats are coughing secondary to asthma it looks like they are trying to get a hairball. Here’s a good video of a cat coughing because he has asthma (click link to see video).
 Jennifer Kim, DVM, DACVIM (Oncology)
Jennifer Kim, DVM, DACVIM (Oncology)
Dr. Kim grew up in New York and received her BA from the University of Pennsylvania in 1998. After spending two years at the National Cancer Institute performing cancer genetic research, she attended veterinary school at Tufts University, graduating in 2003. Dr. Kim completed a rotating internship at the Animal Medical Center in Manhattan, New York and then an oncology internship at Cornell University. She initially began at NorthStar VETS as an emergency clinician in 2005 and returned in January 2010 to treat oncology patients after completing a residency in medical oncology at Michigan State University.
The information presented on this web site is not intended to take the place of your family veterinarian’s advice and is not intended to diagnose, treat, cure or prevent any disease. Discuss this information with your own veterinarian to determine what is right for your pet. All information is intended for your general knowledge only and is not a substitute for medical advice or treatment for specific medical conditions. We can not and do not give you medical advice via this blog. The information contained in this online site and emails is presented in summary form only and intended to provide broad understanding and knowledge. The information should not be considered complete and should not be used in place of a visit, call, consultation or advice of your veterinarian. We do not recommend the self-management of your pet’s health problems.
Posted in Pets, Veterinary Medicine
Tagged anemia, asthma, breathing issues, Cats, dyspnea, feline, Jennifer Kim, NorthStar VETS
Leave a comment
Like a Needle in a Haystack
Bella is a 2-year-old, mixed-breed dog who presented to the emergency service at NorthStar VETS on a referral for swelling in her neck.
She initially presented to her family veterinarian two weeks prior when the swelling was first noticed by her owner. She was treated with antibiotics and the swelling improved, however once the antibiotics were stopped, the swelling returned. Bella seemed to be uncomfortable and have excessive drooling, which promoted her owner to bring her back in for evaluation. Her family veterinarian took X-rays of her neck where the swelling was most prominent. The X-rays revealed evidence of a needle foreign body located deep within the structures of the cervical neck.
Her owner is unsure of where she could have obtained the needle from and was very surprised to hear that this was the cause of Bella’s clinical problem.
 On initial presentation to NorthStar VETS, Bella was seen by our emergency service. Point-of-care bloodwork was taken to make sure Bella was safe for general anesthesia. She was placed under general anesthesia and her neck was clipped to look for evidence of a point of penetration. No wounds or scabs were found. An oral exam was performed and a small hole was noted in the soft palate inside her mouth. The admitting ER doctor, the Dentist and the Surgeons explored this hole, however the needle could not be reached. Given the difficult location of the needle, Bella was taken for a CT scan to obtain a 3-dimensional image. The image helped determine the exact location of the needle by serving as a road map to figure out the best surgical approach possible to retrieve the needle without causing damage to the vital structures of the cervical neck.
On initial presentation to NorthStar VETS, Bella was seen by our emergency service. Point-of-care bloodwork was taken to make sure Bella was safe for general anesthesia. She was placed under general anesthesia and her neck was clipped to look for evidence of a point of penetration. No wounds or scabs were found. An oral exam was performed and a small hole was noted in the soft palate inside her mouth. The admitting ER doctor, the Dentist and the Surgeons explored this hole, however the needle could not be reached. Given the difficult location of the needle, Bella was taken for a CT scan to obtain a 3-dimensional image. The image helped determine the exact location of the needle by serving as a road map to figure out the best surgical approach possible to retrieve the needle without causing damage to the vital structures of the cervical neck.
The CT scan was evaluated by our Radiologist and revealed a needle located at the level of the 2nd cervical vertebra. This proved to be a difficult location to reach without an extensive surgical approach. Therefore Bella was recovered from anesthesia and a surgical team began prepping for surgery the following day. See the 3-D CT scan image of Bella’s neck.
 Bella was given pain medications and antibiotics overnight. She rested comfortably and was ready for her big surgery the following morning. The surgical team consisted of a Surgeon, Neurologist and a Radiologist. Our team worked together to obtain access to this difficult location from the front of her neck under her chin. The needle was buried deep in the muscles and could not readily be identified and therefore our Radiologist used a sterile ultrasound probe to identify the needle. Working together as a team, we were able to make an ultrasound-guided incision into the muscle right over the needle, identify it, and extract it with precision to avoid damage to other structures in the neck.
Bella was given pain medications and antibiotics overnight. She rested comfortably and was ready for her big surgery the following morning. The surgical team consisted of a Surgeon, Neurologist and a Radiologist. Our team worked together to obtain access to this difficult location from the front of her neck under her chin. The needle was buried deep in the muscles and could not readily be identified and therefore our Radiologist used a sterile ultrasound probe to identify the needle. Working together as a team, we were able to make an ultrasound-guided incision into the muscle right over the needle, identify it, and extract it with precision to avoid damage to other structures in the neck.
 Bella recovered well from surgery in our ICU where she was monitored. She did great overnight and was eating, comfortable, and happy the following day. She was discharged into the care of her owner the evening after surgery with antibiotics, pain medications and instructions for warm packing her neck to help the swelling resolve in a timely manner.
Bella recovered well from surgery in our ICU where she was monitored. She did great overnight and was eating, comfortable, and happy the following day. She was discharged into the care of her owner the evening after surgery with antibiotics, pain medications and instructions for warm packing her neck to help the swelling resolve in a timely manner.
 Bella had a recheck two weeks after her surgery to have a physical exam and her sutures removed. We are pleased to report that she is doing great! The swelling in her neck has completely resolved and she is back to her spunky, energetic self. Bella will stay on her antibiotics for another 4 weeks and hopefully will never look back on her run-in with the sewing needle.
Bella had a recheck two weeks after her surgery to have a physical exam and her sutures removed. We are pleased to report that she is doing great! The swelling in her neck has completely resolved and she is back to her spunky, energetic self. Bella will stay on her antibiotics for another 4 weeks and hopefully will never look back on her run-in with the sewing needle.
Penetrating foreign bodies can be challenging cases to diagnose and treat. Most penetrating foreign bodies are very small and difficult to retrieve surgically. As Surgeons, we use the analogy that finding a foreign body at surgery can be similar to finding a needle in a haystack, sometimes impossible. In Bella’s case we were lucky that the offending foreign body could be located with imaging due to its metallic composition. Once we identified and located Bella’s problem, the doctors at NorthStar VETS worked quickly to define a plan of action to retrieve the needle that was located in a very difficult location to access. We assembled a team of doctors each of whom played a part in giving Bella the best chance possible for a positive outcome with minimal surgical trauma. This along with Bella’s strong spirit helped to result in her full recovery.

Heather Knapp-Hoch, DVM, MS, DACVS
Originally from New Jersey, Dr. Knapp-Hoch is excited to return home and join the NorthStar VETS surgical team. Dr. Knapp-Hoch earned her Bachelor of Science in biology from Long Island University in 2001. She then traveled across the US to obtain a Masters degree in genetics and cell and molecular biology from Washington State University where she also obtained her Doctorate of Veterinary Medicine in 2007. Dr. Knapp-Hoch then completed a small animal rotating internship at Cornell University in 2008. Following her internship she completed a three-year surgical residency at Cornell University in 2011. She obtained board certification in 2012 and practiced as a small animal clinical instructor at Cornell University from 2011-2014.
Dr. Knapp-Hoch’s special areas of interest include surgical oncology and minimally invasive surgery including laser ablation of ectopic ureters. She is proficient in advanced wound management and has a special interest in the use of negative pressure wound therapy (NPWT) to treat difficult surgical and traumatic wounds. She is trained in both the tibial plateau leveling osteotomy (TPLO) and the tibial tuberosity advancement (TTA) surgical procedures for cranial cruciate ligament disease.
The information presented on this web site is not intended to take the place of your family veterinarian’s advice and is not intended to diagnose, treat, cure or prevent any disease. Discuss this information with your own veterinarian to determine what is right for your pet. All information is intended for your general knowledge only and is not a substitute for medical advice or treatment for specific medical conditions. We can not and do not give you medical advice via this blog. The information contained in this online site and emails is presented in summary form only and intended to provide broad understanding and knowledge. The information should not be considered complete and should not be used in place of a visit, call, consultation or advice of your veterinarian. We do not recommend the self-management of your pet’s health problems.
Posted in Pets, Veterinary Medicine
Tagged Dr. Heather Knapp-Hoch, Dr. Matthew Gutman, Dr. Melissa Logan, NorthStar VETS
1 Comment
No Cone of Shame Campaign
 E-collars, a medical safety device, are a part of life for dogs and cats undergoing certain procedures here at our hospital. But this month, we’re giving you a chance to turn the “cone of shame” into something beautiful or clever to enhance your pet’s look. If your pet is currently in one of these, has one at home from a previous visit, or if you’re interested in picking one up to participate in this fun competition, then you’re eligible. All you need to do is decorate the e-collar in a most impressive way and submit your images via email to our Marketing Director, Phil Barnes. In your email, be sure to let us know who you are and how to best contact you. We will share your images online via social media as well.
E-collars, a medical safety device, are a part of life for dogs and cats undergoing certain procedures here at our hospital. But this month, we’re giving you a chance to turn the “cone of shame” into something beautiful or clever to enhance your pet’s look. If your pet is currently in one of these, has one at home from a previous visit, or if you’re interested in picking one up to participate in this fun competition, then you’re eligible. All you need to do is decorate the e-collar in a most impressive way and submit your images via email to our Marketing Director, Phil Barnes. In your email, be sure to let us know who you are and how to best contact you. We will share your images online via social media as well.
Get your photo of your pet wearing their decked-out e-collar to us by midnight on Sunday, June 28. From there, we’ll review all the entries and post the best images online where you can vote for your favorite, and you’ll have until midnight on Sunday, July 12 to place your votes (Pet first aid kits are courtesy of MAI).
 We’ll select one dog winner and one cat winner based on the voting results. The winning pet owners will receive a corresponding first aid kit to keep handy at home or while out-and-about with their pet. That’s one winning dog and one winning cat. Good luck and have fun!
We’ll select one dog winner and one cat winner based on the voting results. The winning pet owners will receive a corresponding first aid kit to keep handy at home or while out-and-about with their pet. That’s one winning dog and one winning cat. Good luck and have fun!
Posted in Uncategorized
Leave a comment









 Barbara Maton, DVM, DACVECC
Barbara Maton, DVM, DACVECC M. Joy Weinstein, VMD, DACVS
M. Joy Weinstein, VMD, DACVS